Emily is mum to five children. She’s a qualified midwife working in perinatal mental health in a mother and baby unit.
Hi Emily, thank you for taking the time to talk to me. I’ll admit before speaking to you I had never heard of postpartum psychosis. How is this different from postnatal depression and how common is it?
Thank you for asking me to speak with you! Postpartum psychosis (pp) is a rare but treatable mental health condition that affects 1 in 1000 women in the year following birth more commonly presenting in the first few weeks after having a baby. You are more at risk of developing postpartum psychosis if you have been diagnosed with a bipolar affective disorder or schizoaffective disorder. As many as 1 in 4 women are affected when they have these conditions. This risk rises to 1 in 2 (500 in 1000) if your mother or sister has had postpartum psychosis.
Postpartum psychosis is very different from postnatal depression and it’s characterised by some very scary and distressing symptoms. Including delusions (odd thoughts or beliefs), hallucinations, where you may see things that aren’t there and hearing voices. You may be elated, high and excitable or low mood, withdrawn and unable to care for yourself or baby. Some women experience paranoid thoughts and in extreme cases can feel suicidal or experience thoughts of harm towards their baby or others. Moods thoughts and feelings can change from hour to hour and day-to-day.
Postpartum psychosis is a medical emergency and most women need to be treated in hospital to keep them safe and to recover and the best place for this to happen is in a mother and baby psychiatric unit, where mum can receive specialised treatment and remain with her baby.

Did you have postnatal depression that escalated into postpartum psychosis? At what point did you realise that this could be more than PND? Is postpartum psychosis triggered by something, in which case do you know what triggered yours?
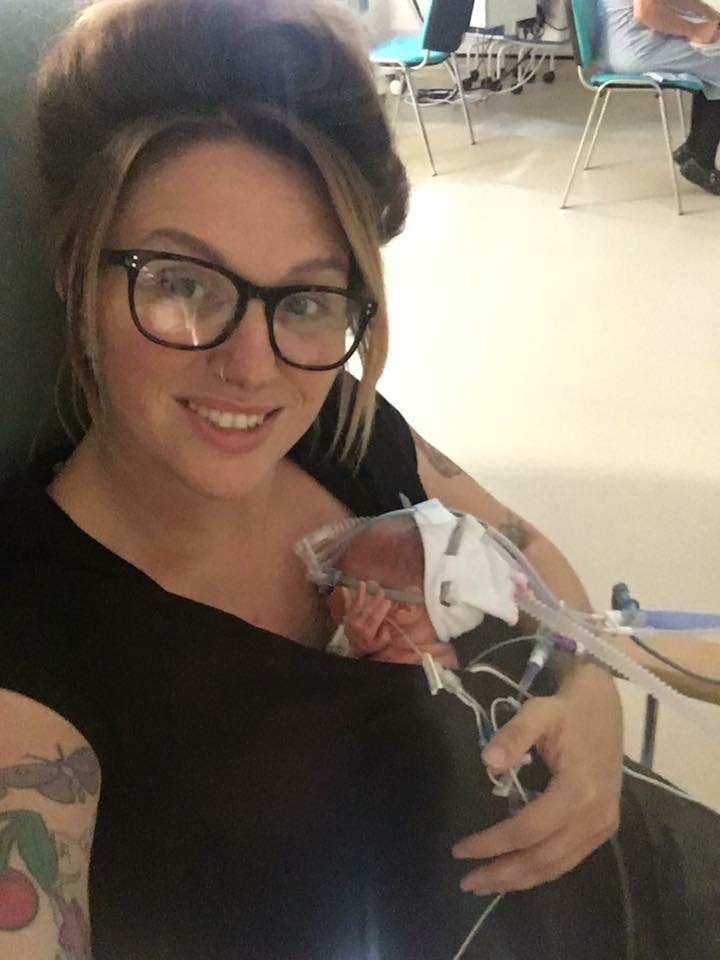
I had experienced low mood, my last child was born at 28 weeks and was subsequently very unwell but I wasn’t diagnosed with PND. Unfortunately, there is no known cause for postpartum psychosis, there are links to hormonal changes following pregnancy and childbirth but other factors are likely to be involved and there is constant ongoing research.
I myself, unfortunately, didn’t realise that I was unwell, my insight into my mental health was clouded because I was already too unwell. My health visitor was able to spot the signs and symptoms and I was subsequently referred to the Crisis mental health team. Postpartum psychosis is an illness that can cause women to become very unwell very rapidly and they themselves would not be able to identify that they were unwell, which is why it is so important that we educate families and health professional about postpartum psychosis, so that they will be able to recognise when their partner, friend, sister or patient is becoming unwell and get the correct help.
You were admitted to a mother and baby unit following your diagnosis, what was this experience like for you? Did you feel supported? How long were you there?
I was admitted to Winchester mother and baby unit (Melbury lodge) in Hampshire and diagnosed with postpartum psychosis. When I was first admitted I was too unwell to recognise my surroundings but I remember feeling scared of the strangers, who were in fact nurses, doctors health care support workers and nursery nurses. I had paranoid and delusional thinking and so until I was stabilised my behaviour was erratic and suspicious.
I was sectioned under the mental health act whilst there as I attempted to escape and needed to be kept safe. It was hard to be away from my family but Melbury Lodge is an amazing place with some very special and caring people working there 24 hours a day. I was supported by all the nursing staff and in particular my named Nursery Nurse. There was always someone to talk to, to provide specialist treatments such as Psychology, along with therapeutic activities that promoted bonding and attachment like baby massage classes and sensory. The staff are so caring and grew to love my son Forrest. They would look after him if I needed to catch up on extra sleep or join in an activity like gardening or an art class.
I was at Melbury lodge for 4 months in total but this also included periods of time when I was able to go home and spend time with my family when I was feeling well. I truly believe that the mother and baby unit saved my life.
Can you begin to express your feelings at the lowest point? Did you hide your feelings or did your friends and family realise something serious was happening?
I had many low points during my illness before I was admitted to the MBU (mother and baby unit) I had attempted to drive into oncoming traffic with my son in the car. I was suffering from command hallucinations in which I was hearing voices that were telling me to kill myself. I felt low and worthless and was convinced that my son and I were going to die. One particularly difficult night in the MBU I attempted to dig my own grave with my hands in the garden. I felt as there was no help for us I had to prepare for our imminent death. The illness had left me feeling a failure.
I had confided to some friends that I was feeling so low before I had become very unwell and they were very supportive and proactive in trying to support me
I’m assuming that as with many other mental health conditions there sadly isn’t a cure. So, how is this controlled? What are the long term effects of suffering from this? Could it return?
It is really important to remember that postpartum psychosis is an incredibly treatable illness and most women will make a full recovery if they receive the right treatment. Treatment options will vary from mother to mother but include medication, psychological treatment such as counselling, therapeutic activities and often SLEEP! Many women with postpartum psychosis will be running on little to no sleep so sleep is often prescribed.
Again, the long-term effects will vary from person to person. I have been diagnosed with Post Traumatic Stress Disorder following my illness and know other mums who have other mental health conditions but equally know women who make a full recovery. Recovery usually takes from around 6-12 months and postpartum psychosis is usually followed by a period of low mood, depression and or anxiety and poor social confidence. Mums are supported in the community by their mental health team.
If you have had an episode of postpartum psychosis your chances of having the illness again rises to around 1 in 2 (500 out of 10000) and can be as high as 7 in 10 for those with a bipolar affective disorder or schizoaffective disorder.

You must have had a lot of questions asked about postpartum psychosis and what you were going through. I should imagine there have also been a lot of comments, some of them hurtful. What would you say has been the most positive thing to come from your experience?
The most positive thing to come from my experience is that I now share what happened to me and my family and help to raise awareness postpartum psychosis, I have been able to speak to health professionals, families and the media alongside other women who have experienced it and this will hopefully ensure that more people are aware postpartum psychosis, the signs and symptoms, how to get help and that recovery is possible! It’s amazing to see the conversations about it and other maternal mental health conditions being opened up, and the changes being made to services because of brave women sharing their stories, and I’m a part of that!
Through advocating for better maternal mental health services I now work at a mother and baby unit just like that one that cared for me 3 years ago as a Senior Nursery Nurse.
You are an advocate for self-care, can you explain to me why that is and why it is so important?
I really believe that self-care is so important as we must remember to take care of our mental health as well as our physical health, because when we become unwell mentally it can have just as much impact on us as if we were to say… break a bone? I’m also a strong believer that self-care doesn’t have to be expensive of following the local trend, it can be a hot coffee, or a magazine in the bath for half an hour, whatever you need to do to take care of yourself. Being a mum means we end up giving our all to our little ones, It’s important to remember who we were before we were parents and also teach our children about self-care and the benefits for their mental health too!
Mummy Social believes that mummy friends are vital during motherhood, have you had support around you during this journey? Have you faced any judgement from those around you? If so how have you dealt with this?
Unfortunately, due to lack of education, fear and sometimes just plain nastiness I have been trolled on the internet for sharing my story. It has been painful at times but it has also encouraged me to continue being so honest, sharing my story is educating people and that in turn will help to break down the stigma surrounding mental health.
I have an amazing group of online friends who have supported me and continue to support me through my journey. I couldn’t have done it without them. It’s important to find your tribe!
Action on Postpartum Psychosis (APP) is the national charity for supporting women and families who are or have experienced postnatal psychosis. They run a peer support service, offer training to health professionals and develop patient information. They are a wonderful resource for support and information. https://www.app-network.org/
Interview by Danni, Mummy Social Team
