Nicky (39) is a mum to names (Mollie, 13, Sadie, 9, Joseph 6) believes she has suffered from pelvic organ prolapse for a number of years, but it became so apparent, last summer, that she needed to seek medical help.
Thank you for taking the time to talk to me Nicky. I understand that you have suffered two prolapses? Could you please briefly explain what this is, how it usually happens and what symptoms you experienced?
I have actually suffered from 3, a bladder (cystocele), bowel (rectocele) and uterine prolapse. Pelvic organ prolapse or POP for short happens when the muscles and tissues supporting the pelvic organs become weak or loose and subsequently one or more of the organs in the pelvis, slip down from their normal position into the vagina.
Some of the symptoms I experienced were:
- A full feeling of heaviness in my pelvic area
- Painful intercourse
- A feeling that something is falling out of my vagina
- I struggled to use tampons and if I did, they would fall out when I stood up.
- Incontinence, both stress and urge
- Constipation
- Low backache
Are there different reasons for prolapses? What is the most common cause? Do you know what caused yours?
Prolapses are caused by weakened pelvic floor muscles and tissue. This could be due to several reasons, for instance:
- Pregnancy
- Difficult labour and delivery or traumatic birth (forceps/ventouse)
- Delivery of a large baby
- Lower oestrogen after menopause
- Chronic constipation or straining with bowel movement
- Chronic cough
- Repeated heavy lifting
I believe mine started during the pregnancy of my first child in 2006. Although I had a relatively easy delivery and average size baby, I had suffered with Polyhydramnios (excess amniotic fluid) and subsequently gained about 5st. This happened with each of my 3 pregnancies and I, therefore, carried a large amount of weight. Stress incontinence was evident after the first of my children and continued to get worse with each.

So , we should all listen to those reminders from the midwife about doing pelvic floor exercises… they are important! Has it been recommended you do any pelvic exercises as part of your recovery?
I am currently doing exercises specific to my recovery, as given by my pelvic health physio, that involves short and longer hold pelvic floor exercises. I am also having to work on my core muscles to build them up again.
When doing pelvic floor exercises, you need to try not to hold your breath or tighten your tummy, bottom or thighs at the same time. You need to tighten the ring of muscle around your front and back passages, drawing the pelvic floor muscle inside. The NHS have an app called Squeezy that other women may find useful too.
I should imagine many women shy away from talking about this subject, I know this is something you’d like to change. Perhaps you could talk us through the impact it has had on your day to day life? Has it stopped you from doing anything that you used to do?
Stress incontinence has been a part of my life for 13 years since my first was born in 2006. I guess I put it down to part of being a mum and accepted that that was how it would be. Some other mummy friends were saying the same thing, so I accepted it as normal. It stopped me from being able to play with them as I would have wanted, I couldn’t jump on a trampoline or even laugh or sneeze without leaking.
When things got really bad last year, I had to stop running which I started to try and get myself a bit fitter and healthier (the Consultant believes that this is what finally made my pelvic floor give way and allow the prolapse out to the entrance of my vagina) I still miss it. I was also reluctant to go out and socialise in case of accidents. It wasn’t something I had discussed with friends as being an issue, it was more joked about more than anything. I also had to advise my place of work about my situation in case I needed to leave class to go to the loo or just the need to sit down (I work in a secondary school). The fear I had that I would empty my bladder in class was at the forefront of my mind and added to my anxiety while dealing with this condition.
My sexual relationship with my partner was also impacted by prolapse. Intercourse became particularly uncomfortable and was not enjoyable due to it, so we therefore stopped. My partner has been so supportive, he’s amazing but I can’t help but feel guilty for the position we’re in.
I also stopped lifting anything particularly heavy, like shopping bags or large loads of wet washing. I may have been overly cautious, but I couldn’t afford for it to get any worse.

Is there a ‘fix’ for a prolapse? What does this involve? Do you have to take medication now? For how long?
In hindsight, I wish I had done my research on the ‘fix’ for prolapse. I saw a private consultant and was advised that I would require surgery in order to rectify the prolapses I had, but I was never given any other options (I probably should have been). I am aware that the new NICE guidelines have been issued with regards to prolapse and I believe that POP sufferers must do a course of pelvic health physio before going for surgery. As frustrating as this may be for some, I think this is a positive move. Depending on the degree of prolapse there are less invasive forms of treatment, such as lifestyle changes. For instance, maintaining a healthy weight or losing weight if you’re overweight; eating a high fibre diet to avoid constipation; avoid lifting heavy objects and avoid high impact exercise like running. Some prolapses can be helped with physio or the use of pessaries. These are devices made from rubber or silicon and inserted into the vagina and left in place to support the vaginal walls and pelvic organs. They can be used to ease the symptoms of moderate or severe prolapses and are a good option if you can’t or would prefer not to have surgery. In my case, a pessary didn’t work as it just dropped back out. There are also side effects to these like discharge, irritation and sores inside the vagina and possible bleeding, urinary tract infections and also, they can interfere with sex. If prolapse has occurred due to lack of oestrogen following the menopause then you can be prescribed synthetic hormones for this.
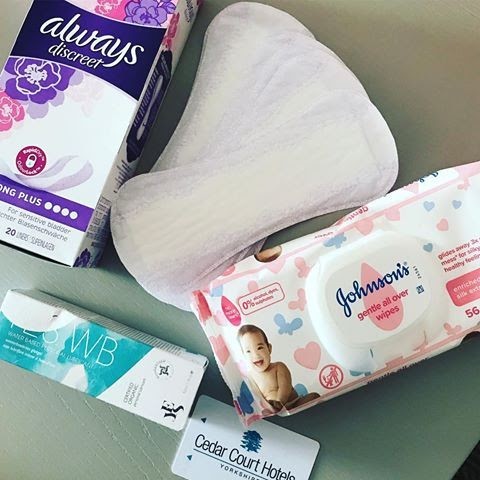
With regards to surgical repair, there are several different types of surgery that involve supporting and lifting the pelvic organs. The type of surgery would depend on the patient and prolapse. The medication involves painkillers after surgery if that is the route you go down, but I am also still taking natural remedies to help with other symptoms that I am now experiencing. I take aloe vera and Dulcoease to help alleviate constipation (a common complaint following hysterectomy), biotin to help aid in growth and strengthening my hair and nails, folic acid as my blood test showed that my folate levels were low, vitamin D to help aid better immunity (a suffered a few infections post-surgery) and finally cranberry to aid better bladder health (again I suffered from multiple UTI’s following surgery). Oh and finally, evening primrose to try and starve off the menopausal symptoms that have started!

I understand that you had a hysterectomy to try and fix your prolapse, how long ago was this? How has your recovery been? How did this make you feel?
I was advised that there was a degree of uterine descent during an initial physical examination and that there was the possibility, that while on the operating table, it could descend further. I wanted to be in control of what happened so, therefore, made the decision to have the hysterectomy before surgery, rather than letting the consultant decide during surgery. This was a massive decision for both myself and my partner as we had planned to have a child of our own together one day (the children we have are from previous relationships) and we had already suffered a miscarriage but in the end, my health took precedence. There are days that I really do struggle with this and the emotion hits me out of the blue.
I had a vaginal hysterectomy and repair in November 2018. I am still recovering now, due to having further surgery in March after suffering another bowel prolapse (due to severe constipation) and skin bridge that needed repairing.
Having all 3 surgeries done at the same time was quite painful. I experienced considerable pain in my vagina for several weeks and my tummy was very swollen and tender too. Emotionally it has been a bit of a roller coaster and I am still trying to come to terms with it. It’s a strange feeling when I know it was my decision to have a hysterectomy, but I still feel a sense of loss. I am currently waiting on some counselling to help come to terms with it.
I was advised to keep my ovaries to prevent me from going into the surgical menopause immediately and I should go into the menopause at roughly the ‘normal’ age. Unfortunately, I have been suffering some of the symptoms of menopause like hair loss, night sweats, hot flushes and fatigue. I am undergoing hormone tests at the moment to try and find out a little more.
Recovery is hard work. They advise you that 6 weeks is the magic number when you will feel better but in reality, it is far from that. As I’ve said, I work in a school, and there was no way that I could’ve gone back to being on my feet all day, at 6 weeks. You need to give your body the best opportunity to be able to heal and if that means taking more time off then so be it. Work have been very understanding, although I have been called in for attendance meetings, but this is all just a case of following procedure. It doesn’t help emotionally though when you’re trying to recover.

Mummy Social believes that mummy friends are vital during motherhood, have you had support around you during this journey?
It’s not just mummy friends, but my mummy! Put it this way, I have certainly found out who my friends are! I couldn’t have done any of this without the support of my family and friends. My mum came and moved in for 6 weeks following both my surgeries, to allow me the best opportunity to heal and recover, as I couldn’t lift anything more than a half-filled kettle, so with a house of 6, it would’ve been impossible. My sister, who’s a mum, has been a great help getting me out of the house, even if it’s just to the local garden centre for a coffee.
My mummy friends, particularly at my kids’ schools, have been amazing support, driving me to and from the shops, carrying my bags and ferrying my children to all their social clubs that they do. I’ve had others just turn up on the doorstep with cake and come and run the hoover over for me and one who is a vet who didn’t hesitate to step in when my dog decided to fill his face with chocolate. These people will never appreciate how grateful I am for all their help and support during the last 6 months. I am sure they must be bored of the continuing saga, but they have never let on. There are some that I haven’t heard from at all too, which is really sad.
Nicky started an Instagram blog to try and aid in her recovery and to get prolapse ‘out there’ to help other women who may be suffering in silence. Please check out @Prolapse_thehiddenshame
Interview by Danni, Mummy Social Team
